HCC Coding Case Study
Overview

Customer: Horizon Healthcare Network, USA

Company: Artigen

Industry: Healthcare

Date:
May 2025
Horizon Healthcare Network, a multi-state provider serving 500,000 patients, faced challenges with manual Hierarchical Condition Category (HCC) coding for Medicare Advantage risk adjustment. Inaccurate coding, missed chronic conditions, and high audit risks led to revenue losses and compliance issues. Artigen’s Cogent AI, an AI-driven HCC coding solution, was deployed to optimize workflows. This case study, aligned with the provided PPT, compares manual versus AI-assisted HCC coding, highlighting transformative outcomes.
Challenges Faced in Manual HCC Coding

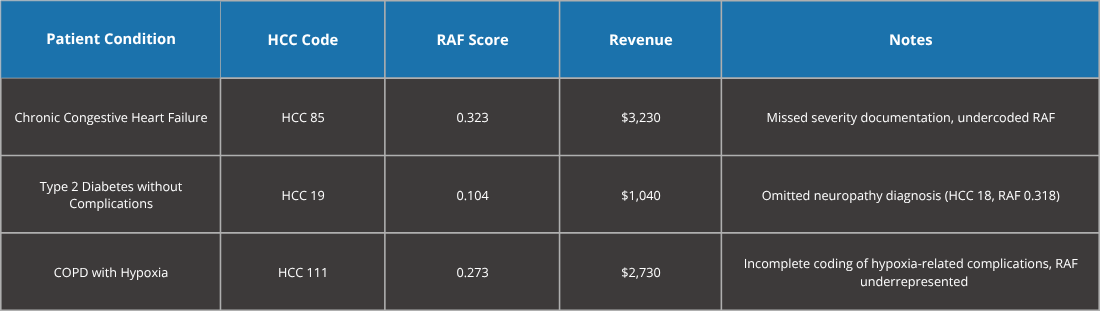
Manual HCC coding required coders to review Electronic Health Records (EHRs), claims, and clinical notes to assign HCC codes and calculate Risk Adjustment Factor (RAF) scores. The process was error-prone, often missing chronic conditions or comorbidities, resulting in lower RAF scores, suboptimal reimbursements, and increased audit risks per CMS guidelines.
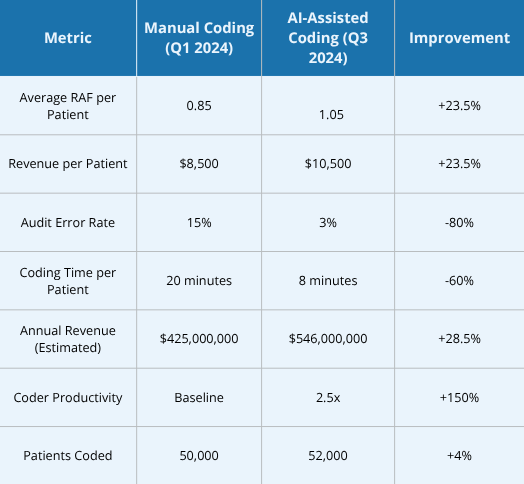
Manual Coding Metrics (Pre-Cogent AI)
- Period Analyzed: Q1 2024
- Total Patients Coded: 50,000
- Average RAF per Patient: 0.85
- Revenue per Patient: $8,500 (at $10,000 per RAF point)
- Audit Error Rate: 15%
- Average Coding Time per Patient: 20 minutes
- Average Coder codes per day: 30
- Annual Revenue (Estimated): $425,000,000
Key Issues:
- Missed HCC codes for chronic conditions (e.g., diabetes with complications).
- Inconsistent comorbidity documentation, lowering RAF scores.
- High audit risks due to non-compliance with CMS guidelines.
- Time-intensive process, reducing coder productivity.
Example Manual Coding Data
Solution: AI-Assisted Coding with Cogent AI
Artigen’s Cogent AI, integrated with Horizon’s EHR and claims systems, leverages NLP and a 3-tier AI model to analyze patient data from EHRs, claims, lab results, and clinical notes. It suggests accurate HCC codes, optimizes RAF scores, and ensures CMS compliance, reducing coder workload and errors.
Implementation Details
- Timeline: Deployed Q2 2024, operational by Q3 2024.
- Training: 2-week coder training on Cogent AI’s interface.
- Integration: Compatible with Epic EHR and claims platforms for real-time coding.
Features
- Data Factory: Integrates EHRs, claims, and lab data.
- AI-Driven Intelligence: Holistically assesses patient profiles for accurate HCC coding.
- Risk Assessment: Identifies chronic and high-risk conditions using advanced algorithms.
- Standard & Custom Reports: Provides insights into patient risk distribution.
- Compliance Support: Aligns with CMS guidelines, reducing audit risks.
- Accuracy Measurement: Continuously improves system and auditor accuracy.
AI-Assisted Coding Metrics (Post-Cogent AI)
- Period Analyzed: Q3 2024
- Total Patients Coded: 52,000
- Average RAF per Patient: 1.05
- Revenue per Patient: $10,500 (at $10,000 per RAF point)
- Audit Error Rate: 3%
- Average Coding Time per Patient: 8 minutes
- Annual Revenue (Estimated): $546,000,000
Key Improvements:
- Comprehensive capture of chronic conditions and comorbidities.
- Reduced audit errors via CMS-compliant coding.
- 60% faster coding, boosting productivity.
- Increased revenue through optimized RAF scores.
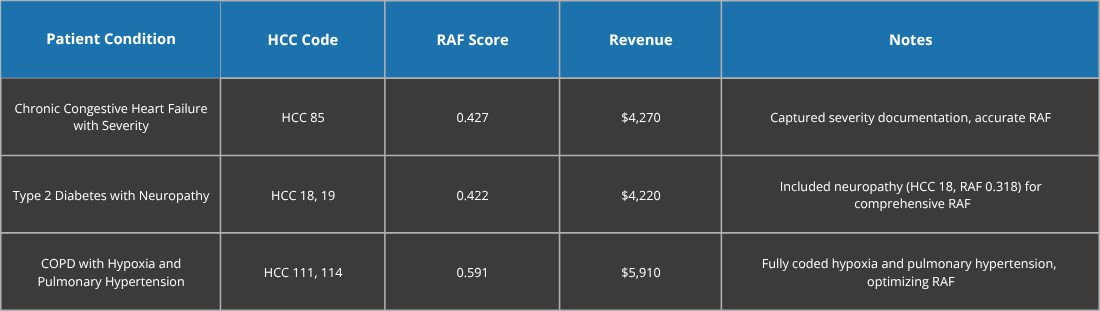
Comparative Analysis
Qualitative Improvements
- Error Reduction: Eliminated undercoding and missed HCC codes (PPT, Page 13: 99% accuracy).
- Coder Satisfaction: Reduced stress with AI guidance, improving job satisfaction.
- Compliance: Lowered audit risks, aligning with CMS regulations (PPT, Page 9).
- Scalability: Handled 4% more patients without additional staffing.
Key Benefits of Cogent AI
1. Precision Coding:
- Accurate HCC code and comorbidity capture, increasing RAF by 23.5% (PPT, Page 13: Efficient Risk Identification).
- Example: Adding HCC 18 for neuropathy increased RAF by 0.318, adding $3,180 per patient.
2. Efficiency Gains:
- Coding time reduced by 60%, enabling 2.5x more cases processed (PPT, Page 13: Productivity beyond 3x).
- Real-time suggestions minimized manual guideline searches.
- Revenue Optimization:
- Revenue per patient increased by $2,000, with $121,000,000 annual uplift (PPT, Page 13: Fair Reimbursement).
3. Compliance and Reduced Audit Risks:
- 80% reduction in audit errors, ensuring CMS compliance (PPT, Page 9: HIPAA Certified).
4. Provider and Coder Empowerment:
- Reduced administrative burden, enabling focus on patient care (PPT, Page 3: Enhanced Care Management).
- Coders gained confidence with AI insights for complex cases.
Net Impact
- Real-Time Coding Support: Enabled concurrent coding, improving accuracy and speed.
- Accurate HCC Mapping: Eliminated errors in code selection and RAF calculations.
- CMS Compliance: Aligned with regulatory standards (PPT, Page 9).
- Coder Productivity: 2.5x increase, freeing resources (PPT, Page 13).
- Revenue Impact: $121,000,000 additional revenue for 52,000 patients.
- Elimination of Audit Friction: Reduced CMS audit corrections.
- EHR Integration: Seamless with Epic (PPT, Page 4: Data Factory).
- Net Revenue Increase per Patient: ~$2,000.
- Time to Close Coding Gaps: 8 minutes per patient, down from 20 minutes.
- Patient Care Enhancement: Accurate risk adjustment improved care coordination (PPT, Page 3).
Conclusion
Artigen’s Cogent AI revolutionized HCC coding at Horizon Healthcare Network, addressing inefficiencies in risk adjustment and revenue cycle management. By improving accuracy, reducing audit risks, and boosting productivity (PPT, Page 13: 99% Accuracy, No Manual Coding), Cogent AI increased revenue by 28.5%, cut audit errors by 80%, and enhanced coder productivity by 150%. The solution’s scalability and compliance focus (PPT, Page 9) position it as a transformative tool for value-based care in the growing U.S. medical coding market (PPT, Page 10: $44B by 2032).